Stacey McHoul left jail last summer with a history of heroin use and depression and only a few days of medicine to treat them. When the pills ran out she started thinking about hurting herself.
“Once the meds start coming out of my system, in the past, it’s always caused me to relapse,” she said. “I start self-medicating and trying to stop the crazy thoughts in my head.”
Jail officials gave her neither prescription refills nor a Medicaid card to pay for them, she said. Within days she was back on heroin — her preferred self-medication — and sleeping in abandoned homes around Baltimore’s run-down Sandtown-Winchester neighborhood.
Thousands of people leave incarceration every year without access to the coverage and care they’re entitled to, jeopardizing their own health and sometimes the public’s.
Advocates for ex-convicts held high hopes for the Affordable Care Act’s Medicaid expansion that promised to deliver insurance to previously excluded single adults starting in 2014, including almost everybody released from prisons and jails.
Many former inmates are mentally ill or struggle with drug abuse, diabetes or HIV and hepatitis C infection. Most return to poor communities such as West Baltimore’s Sandtown, which exploded in violence a year ago after Freddie Gray died from injuries sustained in police custody.
But Maryland’s prison agency, which three years ago said it was “well positioned” to enroll released inmates in Medicaid, is signing up fewer than a tenth of those who leave prisons and jails every year, according to state data. Few other states that have expanded Medicaid under the health law are doing any better, specialists say.
Officials of the Maryland Department of Public Safety and Correctional Services say they do the best they can with limited resources, enrolling the most severely ill in Medicaid while letting most ex-inmates fend for themselves.
“We are battling, every one of us,” to maximize coverage, said prison medical director Dr. Sharon Baucom, pointing to efforts to train sign-up specialists, get Medicaid insurance for hospitalized inmates and share information on mentally ill inmates with other agencies.
“There are handoffs that could be improved,” she said. “With the resources that we currently have, and the process that we have in place, we could do more — and we just need some more help.”
Coverage under Medicaid was seen as an unprecedented chance to transform care for ex-inmates by connecting them to treatment, reducing emergency room visits, controlling disease and putting them on a path to rehabilitation.
As many as 90 percent of people leaving prisons and jails are eligible for Medicaid in states such as Maryland that expanded the federally supported program for low-income residents under the health act, experts estimate. The law gave states the option of extending Medicaid coverage to all low-income adults under 65, not just the children, pregnant women and disabled adults who were mainly included before.
Sickest Inmates Are First In Line
Some 12,000 of Maryland’s 21,000 prison inmates are designated at any given time as chronically ill with behavioral problems, diabetes, HIV, asthma, high blood pressure and other conditions, according to prison officials. But given limited means and the already tall order of connecting emerging prisoners with transportation, shelter and employment, the system focuses on enrolling the very sickest, Baucom said.
“It’s a shame to have to make that call,” she said.
A Double Burden Of Prison And Disease
By Naema Ahmed, Marissa Laliberte, Catherine Sheffo and Daniel Trielli
CAPITAL NEWS SERVICE
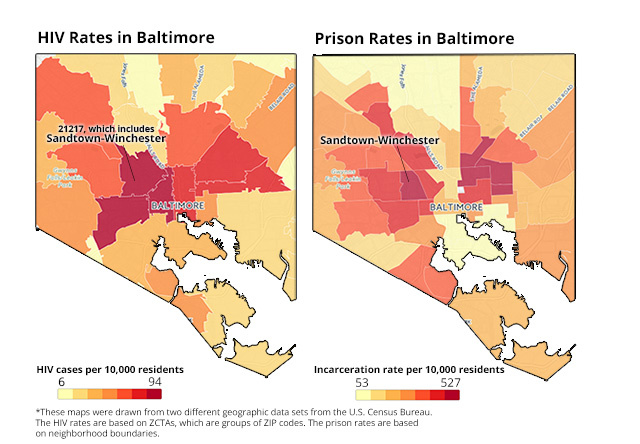
Areas with high incarceration rates also tend to be sicker than average, as shown by HIV and imprisonment data for Baltimore. Linking released inmates to coverage and care could improve public health in these neighborhoods, advocates say.
Sources: Justice Policy Institute, Maryland Health Services Cost Review Commission
Dr. Rosalyn Stewart saw what happened to many chronically ill ex-offenders when she ran a recently completed pilot program to enroll former inmates in Medicaid and get them treatment and shelter.
“People frequently ran out of their medications and did not have access to the care they needed,” said Stewart, an associate professor at the Johns Hopkins University medical school.
McHoul, 40, spent two short stays last year in Baltimore’s Women’s Detention Center. The first time the facility released her without Medicaid coverage. Shortly afterwards she landed in a hospital with an inflamed esophagus. She got out after a second jail stay in August without knowing the hospital had enrolled her in Medicaid between incarcerations, she said.
At neither time did she have more than two weeks’ supply of any medication, including Depakote, a mood stabilizer, she said. For some prescriptions there was less than a week’s store.
“It was whatever was left in the blister pack,” said McHoul, who’s now in a Baltimore drug treatment program. “It’s like, ‘Here’s your supply. Sign this that we gave them to you. See you later.’”
State policy is to give exiting prisoners 30 days’ worth of medicine. But a court ordered McHoul released shortly after she was arrested the second time, which didn’t give the jail enough time to prepare medications, said a corrections spokesman.
There are many Stacey McHouls.
“Maybe somebody needs prescription services and they’re not enrolled and they don’t know where to go,” said Traci Kodeck, interim CEO of HealthCare Access Maryland, a nonprofit that connects consumers to coverage and has worked with the prison system. “Absolutely it happens. Many of them will end up in the emergency departments if we don’t attempt to connect them to services prior to release.”
Mark Pruitt, 46, was released from a Baltimore facility in October with no Medicaid card and a craving for heroin, which he said he had used before he was incarcerated for a parole violation.
He desperately wanted to enter a drug treatment program, but signing up for Medicaid to pay for it was going to take weeks — far longer than he could wait.
“I knew what I wanted. I wanted help,” he said. “I really wanted help. But it’s a struggle when you’re broke — no money, no insurance, feeling defeated. Where do you turn?”
If administrators at a Baltimore recovery facility hadn’t gotten him enrolled in Medicaid, he said, “I think I’d be dead.”
From January 2014, when the Medicaid expansion took effect, through this March, Maryland released almost 16,000 people sentenced to prison or jail, according to state data. Thousands more cycle in and out of jails each year without being convicted.
But the corrections department said it enrolled only 1,337 released inmates in Medicaid from the beginning of 2014 through late March. Another 1,158 prisoners joined Medicaid over that time when they were hospitalized. (Medicaid covers inmates if they spend 24 hours as hospital inpatients; most return to prison.)
Many ex-prisoners are enrolled only when they experience a crisis and end up in an emergency room — the kind of expensive care health officials are trying to reduce. The law requires hospitals to treat emergency cases regardless of insurance coverage. They can retroactively sign those patients for Medicaid.
‘They Don’t Want To Do The Paperwork’
Monique Wright, 35, got out of Jessup Correctional Institution last fall and began suffering acute head and neck pain caused by scoliosis, a spine curvature. Without Medicaid coverage or a doctor, she said she had to seek emergency care at Johns Hopkins Bayview Medical Center.
“It’s the paperwork” that keeps prison officials from making sure people like her have Medicaid upon release, Wright said. “They don’t want to do the paperwork. They don’t have the staff to do the paperwork.”
Advocates wonder why the corrections system is so poor at enrolling what, they often point out, is “literally a captive audience.”
“They’ve had them housed for the past 10, 15 years,” said a frustrated Andre Fisher, a case manager for ex-inmates at Druid Heights Community Development Corp., a nonprofit in West Baltimore. “What’s so hard about it?”
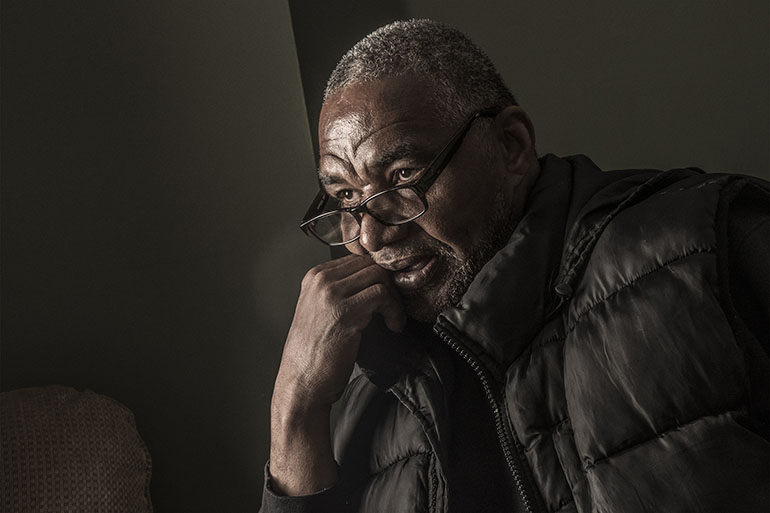
Robert Alston is a house manager at A Step Forward, a Baltimore nonprofit supporting recovering drug users. “Sometimes, you know, the system doesn’t send [ex-inmates] home with that monthly supply” of medicine. “So we have to work rapidly if we come across this.” (Doug Kapustin for KHN)
Enrolling inmates in Medicaid can take weeks, prison officials said. Sometimes the card doesn’t arrive until after they’re out. Computer problems slowed sign-ups in late 2014.
One mistake made by Maryland and most other states is not considering inmates for Medicaid until their release dates approach, said Colleen Barry, a professor at the Johns Hopkins Bloomberg School of Public Health who has studied the process.
“It’s a bad way to do it because you’re getting a very small number” of enrollees by waiting, she said. A better alternative is to enroll inmates when they are booked, as Chicago’s Cook County Jail has demonstrated, she said. Those incarcerated are generally ineligible for Medicaid, but putting them in the system when they enter makes it easier to trigger coverage when they leave, she added.
Ex-Inmates Struggle To Get Medicaid Without Help
If it’s hard for the prison system to enroll inmates, it’s even harder for the individuals to enroll themselves. Those who emerge without Medicaid face a maze of applications, bus trips, phone calls and queues if they want to sign up. Many don’t bother.
For most leaving incarceration, “it’s up to you to go there, make sure you get your health insurance,” said Jamal McCoy, 21, who was living with family in West Baltimore on home detention before he was released. “Most people don’t go. Some people take it easy when they get home.”
Those who try often find that lack of identification is the first challenge. To prevent fraud, Maryland and other states require Medicaid applicants to show verified Social Security numbers.
But jails frequently lose inmate IDs, say prisoners and enrollment officials. Those locked up for years are non-persons for much of the system, with no credit records or driver’s licenses.
That can mean delays of many weeks when released prisoners are especially vulnerable. Gaps in coverage and care of even a few days after fragile patients leave the corrections health system can make the difference between life and death.
“If you’re the diabetic that hasn’t been compliant with your medication, you need your medication now,” said Henrietta Sampson, director of treatment coordination at Powell Recovery Center, a Baltimore addiction recovery agency that works with ex-inmates. “You can’t wait two weeks because you may drop dead.”

Prison officials initiated Medicaid enrollment for William Carter when he was released last year. But doctors told him the program wouldn’t cover an expensive hepatitis C drug until the virus begins damaging his liver. (Doug Kapustin for KHN)
Compared to the rest of the population, ex-prisoners in Washington state were a dozen times more likely to die in the first two weeks after release, according to research by Dr. Ingrid Binswanger, lead researcher for Kaiser Permanente Colorado’s Institute for Health Research. Drug overdose, cardiovascular disease, homicide and suicide were the leading causes of death.
“It’s very important to manage that transition, to make sure people have continuity of care,” she said. (Kaiser Permanente has no relationship with Kaiser Health News.)
Yet in some cases the prison system has stymied outside groups trying to arrange inmates’ coverage. Stewart’s group repeatedly sought permission — “continuously, for about three years,” she said — to meet vulnerable prisoners inside the facility to get an early start on enrollment and post-release appointments. It never happened.
Baucom blamed the problem on “competing priorities” and staff turnover.
Acceptance into Medicaid by the state isn’t the end of the story. Released inmates then must enroll in a private managed-care organization hired by Maryland to provide coverage. That can take weeks longer.
Even when insured, ex-inmates face the same barriers to care experienced by other low-income Baltimoreans — or worse.
Many prison inmates are infected with hepatitis C, which can cause liver damage or cancer over time. But the high cost of curing the disease has prompted Maryland’s and other Medicaid programs to limit access to treatment to those whose livers are already compromised.
“I guess I got to wait until damage is done to my liver,” said William Carter, 50, adding that prison officials initiated Medicaid enrollment when he got out last year.
Released prisoners often have no idea that some Medicaid managed-care contractors allow them to use only certain doctors and pharmacies.
“So a patient goes to Walgreens or wherever to fill something and it’s like, ‘That’ll be $150,’” because he should have gone somewhere else, said Stewart. “They don’t understand what the problem was.”
Even checking all the right boxes sometimes isn’t enough for ex-inmates, who bear the double stigma of poverty and a criminal history.
One released prisoner got an appointment to renew his mental health prescription with a facility in Carroll County, Maryland — his home — that also accepted his Medicaid card, said Baucom. After the clinic learned he had a prison record it cancelled the visit.
“It’s not enough to have a card,” Baucom said. “You’ve got to have access.”
Neighborhoods are at risk when former inmates with chronic illness return.
“You really need to think about this as a public health issue,” said Scott Nolen, director of drug treatment programs for the Open Society Institute–Baltimore, a nonprofit that works on criminal justice policy. “There is transmission of communicable diseases that happens in prison, in confined spaces. And now those folks are coming back into communities, and we want to make sure they get health care.”
In few places is the burden greater than Sandtown-Winchester. Gray, 25, died of spinal injuries that prosecutors filing manslaughter and assault charges blamed on police who arrested him.
The Justice Policy Institute, a nonprofit, called Sandtown “ground zero for the use of incarceration” in Baltimore last year, estimating that nearly one resident in 30 is in prison.
At the same time, three West Baltimore ZIP codes including Sandtown showed the highest rates of HIV infection in Maryland in 2014, according to hospital data from the Maryland Health Services Cost Review Commission obtained and analyzed by Kaiser Health News and Capital News Service.
The corrections department could use more computers, release planners and other enrollment resources, Baucom said.
“If you do the checkoff list, we’ve checked off everything we can do,” she said, noting efforts to increase enrollment capacity and cooperate with the Maryland motor vehicle agency to get inmates state IDs.
Jesse Jannetta, a specialist at the Urban Institute in prisoner re-entry, believes Maryland’s low sign-up rate “is not unusual” in other states. A study published in Health Affairs found prisons and jails nationwide had enrolled 112,520 people in Medicaid from late 2013 up to January 2015, although the authors believe the actual figure was higher.
Federal and state prisons released 636,000 people in 2014, according to the Justice Department. Millions more are estimated to cycle through jails each year.
Few independent experts expect Maryland — let alone most other states — to come anywhere close to full enrollment of emerging inmates anytime soon.
“It’s fair to say we’re just at the tip of the iceberg” in prisoner enrollment, said Johns Hopkins’ Barry, a coauthor of the Health Affairs study. “Maryland is always an innovator. If Maryland is still at the cutting edge of how to do this, many areas of the country don’t have any of these types of programs in place.”
This article was reprinted from kaiserhealthnews.org with permission from the Henry J. Kaiser Family Foundation. Kaiser Health News, an editorially independent news service, is a program of the Kaiser Family Foundation, a nonpartisan health care policy research organization unaffiliated with Kaiser Permanente.
This story is a partnership with The Baltimore Sun and Capital News Service, which is run by the University of Maryland’s Philip Merrill College of Journalism. KHN reporter Shefali Luthra and CNS reporters Catherine Sheffo, Daniel Trielli, Naema Ahmed and Marissa Laliberte contributed.